Exploring the Various Types of Ankle Fractures
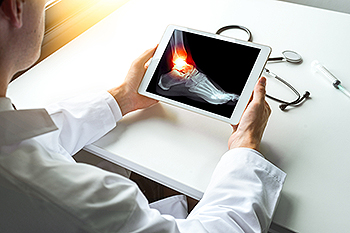
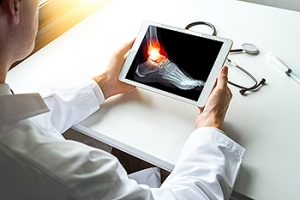
When it comes to ankle injuries, fractures are a common concern. Broken ankles can encompass several types of fractures, each with distinct characteristics and implications. One of the most frequent fractures is the lateral malleolus fracture, which occurs on the outer bone of the ankle. This type is often linked to a sudden twisting or rolling of the foot. Medial malleolus fractures, on the inner bone of the ankle, can result from severe impacts of excessive stress on the inside of the ankle joint. High ankle fractures, known as syndesmotic fractures, involve the ligaments that connect the tibia and fibula. These are typically caused by high-impact injuries and are often more complex to treat. Understanding the type of ankle fracture you have is essential for proper diagnosis and treatment. The symptoms and recovery process can vary, making it vital for podiatrists to assess the injury accurately and recommend appropriate care. Regardless of the fracture type, prompt and effective treatment is essential for optimal healing and a faster return to a pain-free, functional ankle. If you have broken your ankle, it is suggested that you consult a podiatrist who can determine what type of fracture it is, and offer appropriate treatment methods.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from The Podiatry Center, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Broken Ankles
Broken ankles are a serious injury that can lead to an inability to walk, function, and also cause a significant amount of pain. A broken ankle is a break in one of the three bones in your body that connect at the ankle joint: the tibia, the fibula, and the talus. The tibia and fibula are your two primary leg bones that connect at the knee, which sit directly upon the talus bone. This is protected by a fibrous membrane that allows for movement in the ankle joint. A broken ankle is usually caused by the foot rolling under or twisting too far, causing one of these three bones to snap.
A broken ankle is different from an ankle sprain, which occurs when the ankle ligaments are ripped or torn but no bones have been broken. A sprain can still be very severe, causing bruising in the foot and an inability to hold your own weight, much like a broken ankle would. If you’re unable to stand, and suspect that you have a broken ankle, the first thing to do would be to get an immediate X-ray to determine the severity of the break.
A common cause of broken ankles is when the ankle is rolled over with enough pressure to break the bones. This usually happens during exercise, sports, or other physical activity. Another common cause is a fall or jump from a tall height.
One immediate treatment for pain relief is elevating the foot above your head to reduce blood flow to the injured area. You can also apply ice packs to your ankle to help reduce swelling, redness, inflammation, and pain. After these initial steps, getting a cast and staying off your feet as much as possible will aid in the recovery of the broken ankle. The less movement and stress the ankle has to endure, the more complete it will heal. A doctor can determine if surgery is needed in order to heal correctly. In these cases, an operation may be the only option to ensure the ability to walk properly again, followed by physical therapy and rehabilitation.
It is highly important to determine if surgery is needed early on, because a broken ankle can become much more severe than you realize. If not professionally treated, the broken ankle will inhibit your walking, daily functioning, and produce a large amount of pain. Treating your broken ankle early on will help prevent further damage to it.
Managing Diabetic Neuropathy

Diabetic neuropathy, a consequence of prolonged elevated blood sugar levels in individuals with diabetes, affects up to 50 percent of those with the condition. Symptoms of diabetic neuropathy range from pain, tingling, and numbness in the extremities to potential onset without noticeable signs. Peripheral diabetic neuropathy is prevalent, causing discomfort in the toes, feet, and hands. Early diagnosis is essential, and a thorough examination by a podiatrist is suggested. This process can include a foot check for sores and ulcers, along with tests such as the monofilament test, nerve conduction tests, and electromyography. Effective management of diabetic neuropathy involves strict control of blood sugar levels through regular monitoring, adherence to an antidiabetic diet, physical activity, and routine blood pressure checks. Medications can also play a vital role in relieving symptoms. If you have diabetes, it is suggested that you are under the care of a podiatrist can help you to manage this condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from The Podiatry Center, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
How Seniors Can Prevent Falling

As people age, preventing falls becomes more and more important for maintaining overall well-being. Exercise plays a pivotal role in fall prevention. Activities that improve balance and strengthen your legs, such as Tai Chi, are beneficial. Lack of exercise leads to weakness, increasing the risk of falls. Regular eye and foot check-ups are essential, as poor vision raises fall risks. Certain modifications can enhance your safety at home. Remove tripping hazards, secure rugs with double-sided tape, and place frequently used items within easy reach. Install grab bars in the bathroom, use non-slip mats, and improve lighting. Lastly, wear well-fitting, supportive shoes, both indoors and outdoors. Handrails and proper lighting on staircases, both indoors and outside, contribute to a safer living environment. Review all medications, as some can cause dizziness. Discuss vitamin D supplements to enhance bone, muscle, and nerve health. Keep your podiatrist informed if balance or other foot problems are putting you at risk for falls. Additionally, it is suggested that you schedule an appointment yearly to have your feet examined by a podiatrist in addition to discussing any foot issues that may contribute to risks of falling.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from The Podiatry Center, PC. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Older Women Are More at Risk for Bunions

Hallux valgus, commonly known as a bunion, is a prevalent foot condition that affects many individuals, especially as they age. A bunion is characterized by the big toe bending towards the smaller toes, accompanied by a painful bony protrusion at the inside of the foot. Recent research shows the prevalence and factors associated with hallux valgus in an older adult population, and women in particular. The study revealed that the prevalence of bunion deformity was higher in women and increased with age. Family history, wearing high-heeled or narrow shoes, and having flat feet were identified as contributing factors. The severity of hallux valgus also significantly affected participants' quality of life. Additionally, participants reporting foot pain in the previous 12 months showed higher scores in both pain and decreased function, highlighting the substantial impact of bunions on daily activities. This research emphasizes the importance of proactive foot care, especially for older women who are more susceptible to the formation of bunions. Regular check-ups with a podiatrist, appropriate footwear choices, and early intervention can play an important role in preventing and managing this foot deformity. For help in managing the pain and side effects of bunions, it is suggested that you schedule an appointment with a podiatrist for the appropriate treatment option.
If you are suffering from bunions, contact one of our podiatrists of The Podiatry Center, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.