Connect With Us

Causes and Symptoms of a Broken Pinky Toe

A broken pinky toe, or 5th phalangeal fracture, can occur due to various reasons such as stubbing the toe against furniture or dropping something heavy on it. Symptoms typically include immediate pain, swelling, bruising, and difficulty in moving the toe. Types of fractures can range from minor hairline cracks to complete breaks that displace the bone. Stress fractures develop gradually from repetitive stress, while traumatic fractures occur suddenly from impact or trauma. Diagnosing a broken pinky toe involves a physical examination and possibly imaging tests like X-rays to determine the extent of the injury. Treatment usually involves rest, elevation to reduce the swelling, and buddy taping the toe to its neighbor toe for support. Severe fractures may require immobilization with a splint or walking boot, and in rare cases, surgery to realign the bones for proper healing. If you have endured a broken pinky toe, it is suggested that you consult a podiatrist who can provide you with the appropriate treatment method.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact one of our podiatrists from The Podiatry Center, PC. Our doctors will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
- Swelling
- Pain (with/without wearing shoes)
- Stiffness
- Nail Injury
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
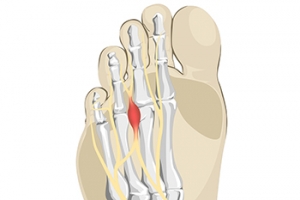
Definition and Incidence of Morton’s Neuroma
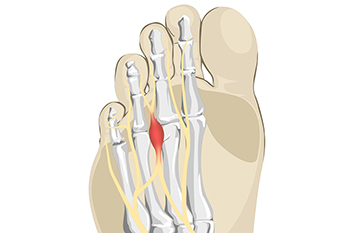
Morton's neuroma is a painful condition affecting the nerves between the toes, most commonly the third and fourth toes. It involves a thickening of the tissue around one of the nerves leading to the toes, causing sharp, burning pain or a sensation of stepping on a pebble. This benign growth, also known as intermetatarsal neuroma, results from repeated stress or irritation, often due to activities that involve wearing tight shoes or high heels. The incidence of Morton's neuroma varies, affecting more women than men, and typically occurring between the ages of 30 to 50. It involves the interdigital nerves becoming compressed or irritated, leading to inflammation and discomfort. If you have pain between these toes, it is suggested that you seek counsel from a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of The Podiatry Center, PC. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Foot Pain May Be Linked to Falls in the Elderly
 Foot pain is a significant factor contributing to falls in seniors. Research indicates a link between severe foot pain and a higher incidence of recurrent falls in older adults. Conditions like arthritis, plantar fasciitis, bunions, and flat feet can cause pain that affects balance and gait. Flat feet, in particular, can lead to altered foot mechanics, increasing the risk of falling. A podiatrist can be instrumental in preventing falls by addressing these issues through regular foot examinations. This foot doctor can diagnose and treat foot conditions, as well as recommend supportive footwear and prescribe orthotic inserts. They can also provide pain management strategies and suggest personalized strength training and foot exercise programs that improve stability and mobility. If you are 65 years of age or older and have fallen in the last year as a result of foot pain, it is suggested that you schedule an appointment with a podiatrist for an exam and suggested fall prevention measures.
Foot pain is a significant factor contributing to falls in seniors. Research indicates a link between severe foot pain and a higher incidence of recurrent falls in older adults. Conditions like arthritis, plantar fasciitis, bunions, and flat feet can cause pain that affects balance and gait. Flat feet, in particular, can lead to altered foot mechanics, increasing the risk of falling. A podiatrist can be instrumental in preventing falls by addressing these issues through regular foot examinations. This foot doctor can diagnose and treat foot conditions, as well as recommend supportive footwear and prescribe orthotic inserts. They can also provide pain management strategies and suggest personalized strength training and foot exercise programs that improve stability and mobility. If you are 65 years of age or older and have fallen in the last year as a result of foot pain, it is suggested that you schedule an appointment with a podiatrist for an exam and suggested fall prevention measures.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from The Podiatry Center, PC. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Causes and Prevention of Ankle Pain While Cycling

Ankle pain while cycling is often due to poor form, overtraining, or using a bike that is the wrong size. Improper cycling form, such as incorrect foot positioning on the pedals, can strain the ankle joints and muscles. Starting with intense or prolonged rides too quickly without allowing your body to adapt can also lead to overuse injuries, including ankle pain. Additionally, riding a bike that does not fit your body properly can force your ankles into awkward positions, causing discomfort and potential injury. To prevent ankle pain, focus on maintaining correct form by keeping your feet properly aligned on the pedals. Gradually increase the intensity and duration of your rides to build strength and endurance. Additionally, ensuring your bike is properly fitted to your body can also help maintain proper alignment and reduce the risk of ankle pain. If your ankle begins to hurt during or after a bike ride, it is suggested that you consult a podiatrist who can properly treat it, and guide you on additional ankle injury prevention techniques.
Sports related foot and ankle injuries require proper treatment before players can go back to their regular routines. For more information, contact one of our podiatrists of The Podiatry Center, PC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are a common occurrence when it comes to athletes of any sport. While many athletes dismiss the initial aches and pains, the truth is that ignoring potential foot and ankle injuries can lead to serious problems. As athletes continue to place pressure and strain the area further, a mild injury can turn into something as serious as a rupture and may lead to a permanent disability. There are many factors that contribute to sports related foot and ankle injuries, which include failure to warm up properly, not providing support or wearing bad footwear. Common injuries and conditions athletes face, including:
- Plantar Fasciitis
- Plantar Fasciosis
- Achilles Tendinitis
- Achilles Tendon Rupture
- Ankle Sprains
Sports related injuries are commonly treated using the RICE method. This includes rest, applying ice to the injured area, compression and elevating the ankle. More serious sprains and injuries may require surgery, which could include arthroscopic and reconstructive surgery. Rehabilitation and therapy may also be required in order to get any recovering athlete to become fully functional again. Any unusual aches and pains an athlete sustains must be evaluated by a licensed, reputable medical professional.
If you have any questions please feel free to contact our office located in Millburn, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sports Related Foot And Ankle Injuries
Foot and ankle injuries are common among people who participate in sports. Several factors contribute to this. They include failing to stretch or warm up properly, not wearing the proper type of shoe and not taping or providing other types of support for the ankle or foot. The most common foot and ankle injuries suffered by people involved in sports are plantar fasciitis, ankle sprains and Achilles tendon damage or ruptures. If not treated properly, they can lead to permanent disability.
Treating these injuries is relatively simple if they are identified and addressed early. Many athletes dismiss the initial aches and pains associated with injury as just soreness or tired muscles. Their first response is usually to try to work through it. This can lead to serious problems. Many minor injuries are made far more serious when athletes continue to put strain and pressure on them. That attitude can change a mild strain into a serious strain and a minor tear into a rupture. Athletes should have unusual aches and pains evaluated by a skilled medical professional.
Plantar fasciitis is a painful injury. It is inflammation of the plantar fascia, the thick band of tissue running from the heel to the base of the toes. If left untreated, it can lead to a degenerative disease called plantar fasciosis. There are several effective treatments for this ailment. Doctors often prescribe rest, massages, stretching, night splints, physical therapy, anti-inflammatory medication, corticosteroids or surgery, usually in that order. The most effective treatment for plantar fasciitis is orthotics, which offers foot support. Surgery is occasionally used as a last resort, but it comes with the risk of nerve damage and infection and often does not stop the pain.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone. Running, jumping and walking all impact this tendon. Two common injuries to the Achilles tendon are tendonitis and a rupture of the tendon. Tendonitis is inflammation in the tendon often caused by an increase in the amount of stress placed on it. Non-surgical treatments include rest, ice or anti-inflammatory medication. A rupture (tear) of the Achilles tendon can be treated by placing the lower leg in a cast for several weeks or with surgery. Many physicians feel surgery is the better option because it lowers the risk of re-ruptures. Both methods require 4 to 6 months of rehabilitation.
Ankle sprains are the most common sports related foot and ankle injury. A sprain occurs when the ligament holding the ankle bones and joint stretches beyond its normal range. It can be treated non-surgically with a combination of rest, ice wrapped around the joint for 30 minutes immediately after injury, compression by a bandage and elevating the ankle above the heart for 48 hours. This combination is referred to as RICE. Severe ankle sprains in which the ligaments are torn may require reconstructive surgery followed by rehabilitation.
Are Bunions Affecting Your Everyday Life?
Blog Archives
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016
- December 2015
- November 2015
- October 2015
- September 2015
- August 2015
- July 2015
- June 2015
- May 2015
- January 2014
- December 2013
- November 2013
- October 2013
- September 2013
- August 2013
- July 2013
- June 2013
- May 2013
- April 2013
- March 2013
- February 2013
- January 2013
- December 2012
- November 2012
- October 2012
- September 2012
- August 2012
- July 2012
- June 2012